Commonly Asked Questions about the VGDS – For Private Providers
Please find the most asked questions and answers regarding the Victorian General Dental Scheme below.
If you can't find the answer to your question, please contact us by:
Email: vicdental@dhsv.org.au
Phone: 03 9341 1700
Victorian General Dental Scheme - Practitioner Item Schedule
Victorian Privately Contracted Dental Schemes - Provider Handbook
On behalf of the Victorian Government, Dental Health Services Victoria (DHSV) purchases dental services from Community Dental Agencies (agencies) for eligible Victorians. Most of these services are provided by public dental providers, with a proportion also provided by private providers.
The VGDS voucher may be offered to patients on public General waiting lists, particularly where community dental agencies do not have the capacity to provide in-house care, or where additional funding is available.
Any private provider, registered with the Dental Board of Australia, may participate in the scheme.
It is not necessary for a private dental provider to sign a formal contract in order to participate in privately delivered schemes. Treating a patient (issued with a voucher) and subsequently submitting a claim for payment is taken as agreement to adhere to scheme guidelines. Providers may participate in privately delivered schemes on a case-by-case basis.
The following groups, being eligible for public dental services, may have their treatment provided via vouchers:
- People aged 18 years and over, who are health care or pensioner concession card holders or dependents of concession card holders
- All Aboriginal and Torres Strait Islander peoples
- All Refugees and Asylum Seekers.
For people aged 18 years and over, who are health care or pensioner concession card holders or dependents of concession card holders
- The patient’s concession card should be sighted, with a valid date as at the date of issuing the voucher.
- It is suitable to complete treatment where a patient’s concession card is not being renewed by Centrelink but was valid as at the issue date of the voucher.
- Where a patient presents with a voucher and eligibility cannot be confirmed, treatment should not be provided until confirmation of eligibility is received; contact should be made with the authorising agency for advice.
For Aboriginal and Torres Strait Islander peoples, and Refugees and Asylum Seekers
- Presenting with a valid voucher is sufficient evidence that they are eligible.
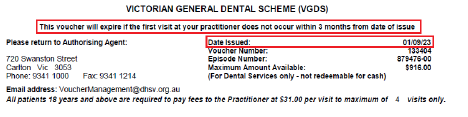
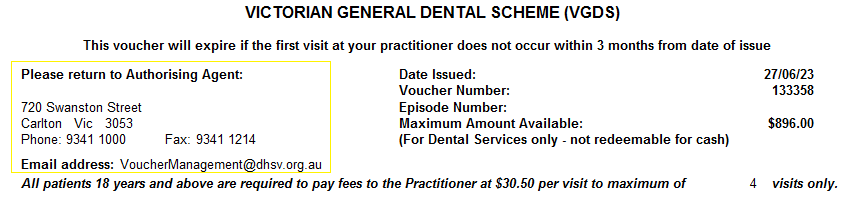
Should a client be required to pay any co-payment, this will be clearly indicated on the voucher.
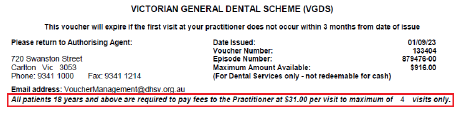
For fee paying clients, general dental care costs $31 per visit, for the first 4 visits (i.e maximum of $124.00).
If they need more visits after this, they no longer need to make a payment. The visits are shown at the top of the voucher.
The VGDS has a defined schedule of services, defined by the ADA Inc. Australian Schedule of Dental Services and Glossary, 12th edition. Remuneration for services provided by participating providers is based on the Department of Health State Rate Fees for Private Schemes. For more information please visit - Access to Victoria’s public dental care services (health.vic.gov.au).
- A VGDS voucher is valid for 3 months from the date of issue.
Clients presenting with expired vouchers should be redirected to the authorising agency. The authorising agency will advise them of their next steps
- Practice Details: Please fill in this section clearly, so we have correct details to send you payment.
- Please make sure to only use the item numbers on the VGDS item schedule.
- Please make sure to add the tooth number treated and also the surface where applicable.
- The client needs to sign this voucher when their treatment is completed, and before you send it back to us. This is the last section of the voucher. This shows the client has agreed to treatment and confirms what they have had completed and what they have paid.
- The clinic then also signs. Any vouchers returned without the patient declaration signed off will be returned for completion.
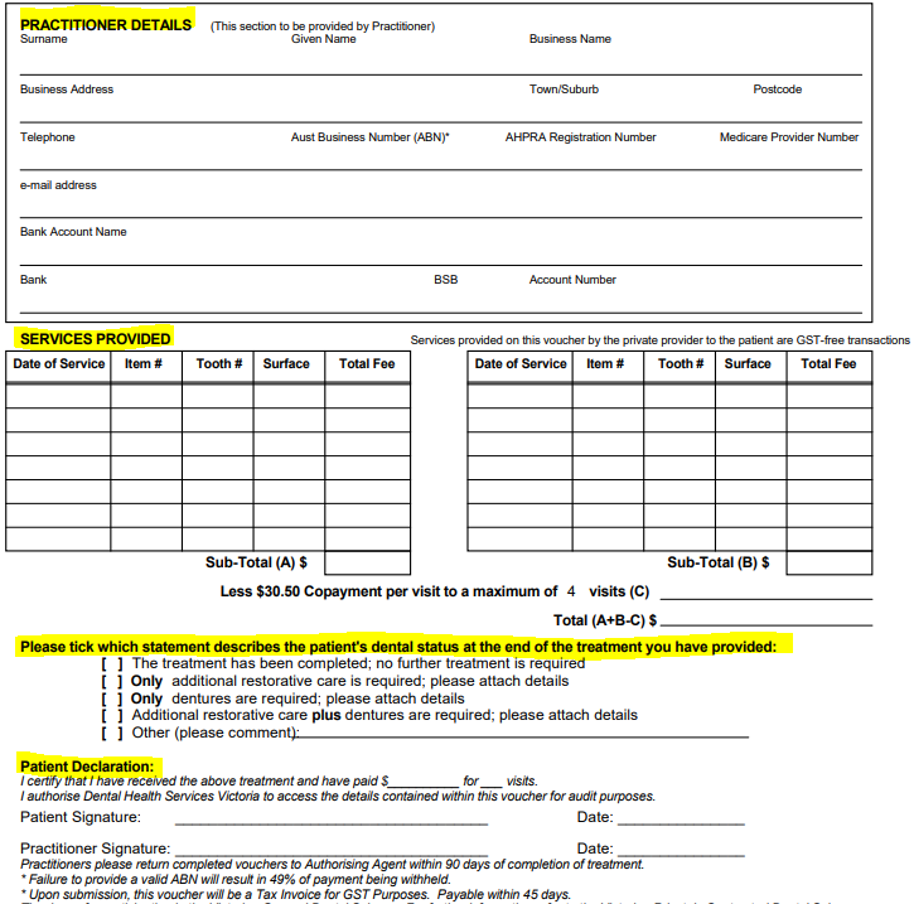
Return the voucher within 90 days of treatment completion to the authorising agency. The authorising agency’s information can be found on the top left-hand corner of the voucher.
Payment of claims will be made within 45 days of the voucher being received by the agency. All queries regarding reimbursement of claims should be directed to the agency identified on the voucher.
The maximum amount available through the VGDS voucher is $916. This amount is inclusive of the client co-payment fees. The amount you will be paid will be $916 minus the client's contribution. Please do not go over this amount, we can only pay up to this per voucher.
Please add up the fee costs from treatment and then subtract how much the client has paid to you. It is advised to keep tab of the treatment and the costs as you as you do not go over the capped amount.
Any patient co-payments cannot be claimed against private health insurance.
Example:
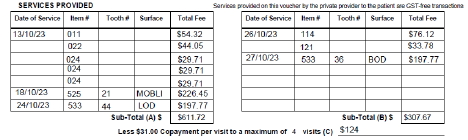
In this example the client has had 5 visits (13/10/23, 18/10/23, 24/10/23, 26/10/23 and 27/10/23).
- Of the 5 visits, the client has paid 4 lots of co-payment fees of $31(as indicated on the voucher) which is a total of $124.
- The client has received treatment costing $919.39 which is above the maximum amount available ($916).
Therefore, the private provider will be paid $916 minus $124, which is $ $792 from the authorising agency.
Given the capped limit for each voucher, private providers are encouraged to provide all or as much of the most urgent dental care required for each patient within the scope of this limit. Additional voucher(s) may be made available for completion of care, or more complex care may be provided at the agency.
If the client requires additional treatment, please complete the first voucher (keeping to the total amount) and send that back to the authorising agency with a proposed treatment plan with relevant items codes.
The authorising agency will review this information and get back to you and the client with the next steps.
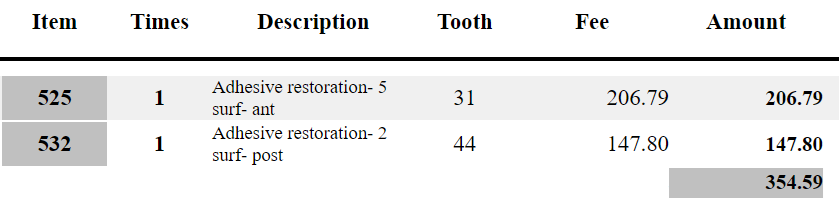
Here is an example of a proposed treatment plan:
Submissions of items not contained within the schedule or beyond the voucher cap may not be reimbursed.
If the client wishes to proceed with treatment of items not contained within the VGDS item schedule they can cover the cost out of their pocket. This would be agreed between you and the patient.
Alternatively, please refer them back to their local community dental agency. Please give the following information to the client, so a suitable clinical handover can take place:
- Treatment plan
- A summary of treatment carried out with diagnostic tests and radiographs (these may be requested for further treatment; you could consider double films)
Contact the authorising agency that has issued the voucher and let them know. They will advise you of your next steps.
Please contact the authorising agency OR Dental Health Services Victoria (DHSV) on vicdental@dhsv.org.au or(03) 9341 1700.